Making dollars & sense from Transparency in Coverage MRFs
Phantom prices, ghost providers, and ghoulish implications
In effort to increase healthcare transparency and empower consumers to make informed decisions, the Transparency in Coverage (TiC) rule was finalized in 2020 by the Depts of Health & Human Services, Labor, and the Treasury, requiring health plans to disclose negotiated prices for medical services, releasing Machine Readable Files (MRFs) for payments by procedure and provider beginning 7/1/22.
As stakeholders wade into massively complex MRFs arriving on monthly loop, what is readily apparent is the significant presence of “ghost providers” listed at “phantom prices.”
These are lines of data in the files that look like all the others, but designate providers by NPI listed for services they do not perform at prices they have not and will not be reimbursed at.
In other words, there’s more “trick” than treat. Perhaps if these erroneous prices largely matched real rates, this would not be a major issue. Unfortunately, in many cases, they do not.
Lumbar Discectomy in New York City
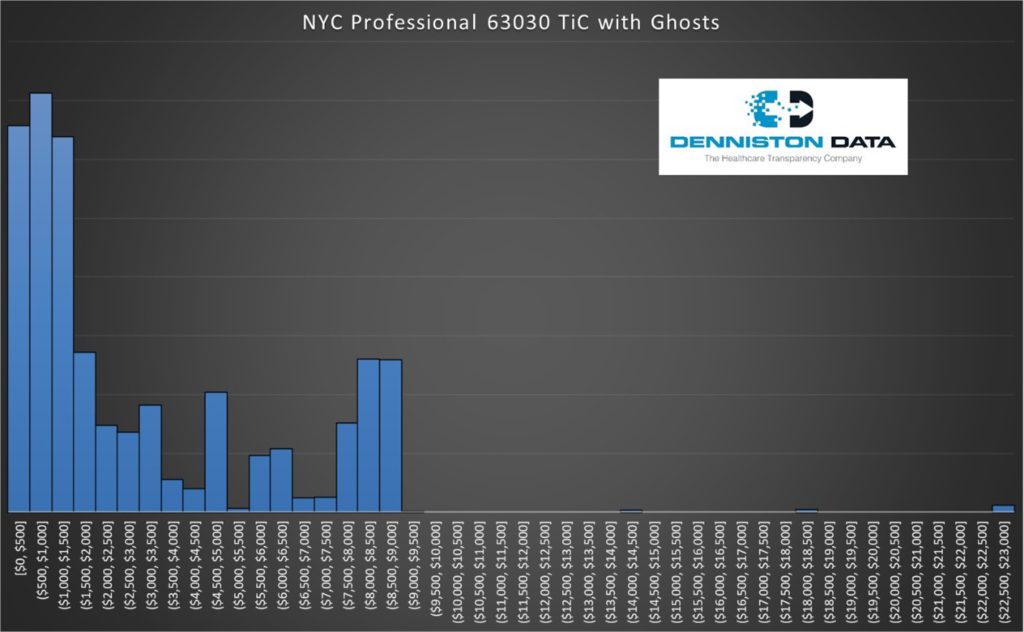
Let’s review an example. For stakeholders using the TiC data across five major health plans in New York City (Aetna, Anthem, Cigna, Surest, UnitedHealthcare), without any mechanism to exclude ghost providers, the revealed rates for a low back discectomy are as follows-
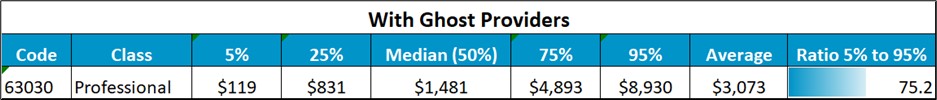
This data suggests (a) huge variability in reimbursement rates, a 75x multiple from the 5th percentile to the 95th percentile, and more than 5x even from the 25th percentile to the 75th, and (b) the fair market reimbursement in NYC appears to be about $1,500 – $3,000 (median to average).
Now, how much of that is true?
Turns out, very little. When we filter the TiC data for prices using only providers that regularly perform and bill for discectomies, we get wildly different results-
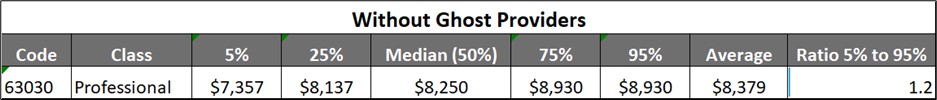
The real story is much less variability, with NYC reimbursement rates of about $7,000-$9,000.
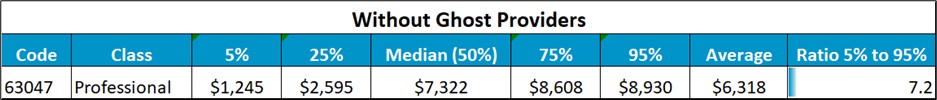
Interestingly, removing ghosts doesn’t typically drop variability that much, as for 63047 (laminectomy), even without ghosts we find a much wider range-
The first step in TiC analysis is to always remove trick from treat.
There are several ways to attempt to remove phantom prices. The most common is to use taxonomy codes, but these can still leave ghosts lurking in your dataset. For example, selecting for Orthopaedic Surgery doesn’t tell you which orthopods focus solely on backs vs knees vs shoulders. Secondly, it can also exclude real rates from other providers that may register differently, for example, Sports Medicine.
To get to that specificity, utilization data is needed – what providers do and are being paid for at the code level. We do that here at DDI given our focus on physician quality, ranking physicians by what they do most and are good at (PRS), and healthcare pricing (HPG) with our transparency solutions.
Price vs Quality
Interestingly, while quality and price are intertwined, they are not nearly as correlated as one would expect. Some of the best physicians and specialists may be priced lower, while others of equal or lesser quality may see reimbursement of 2, 3, even 5x. It’s not unusual to find multiple providers within a few miles of each other of largely similar quality, but wildly different in reimbursement rates.
Using Laminectomy in NYC and selecting for a single payer, UHC, we find the distribution as follows-
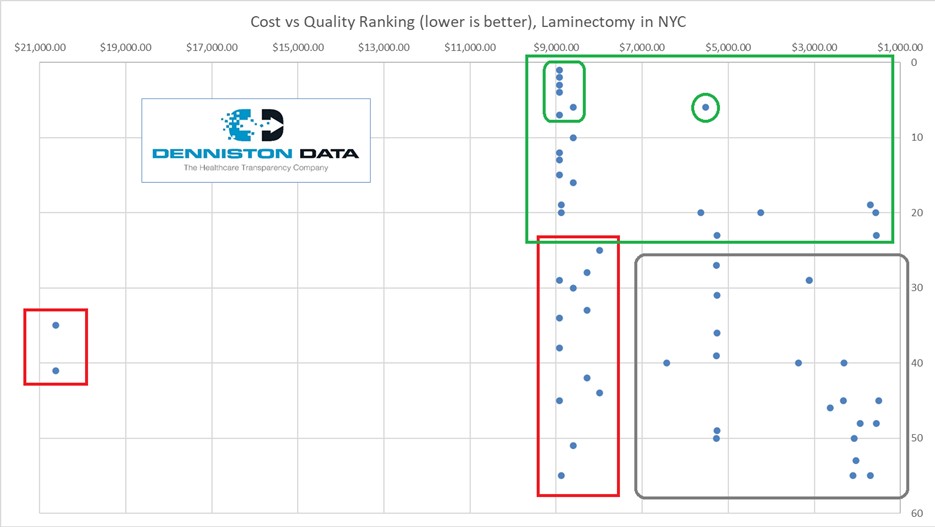
Nearly all the “best” – top 10 – providers and practices in the UHC network charge about $9k for the laminectomy, but one stands out at considerably less, about $5,500. If we widen to the top 20 providers and practices, we find options at much lower prices, still among higher ranked providers.
For back surgery, where experience is critical, any doctor in the green box is a great choice, especially those that are circled.
Those in the red boxes (especially the one on the left) should be our last choice for specialty referral by concierge or to steer members via their doctor-finder portals.
The two on the far left are charging about $20,000 each and are not among the most experienced. There’s a bunch at market prices ($8k-$9k), but for the same price, you’d rather use the upper tier for quality, or pay a lower price in the gray box for similar expectations around quality.
What we pay is price, but what we get is value, and that equation must consider quality.
The correlation of price to quality here is about 0.27, which is considered weak. That means there are huge opportunities in healthcare to select high quality physicians at more reasonable prices.
Implications of Misleading TiC Data
Back to price, given the difference in reported costs when cross-checked against utilization data, most of the prices in the NYC TiC files are not likely to be “real”. Here’s another visual-
The real story, without the ghosts, looks more like this (boxed area)-
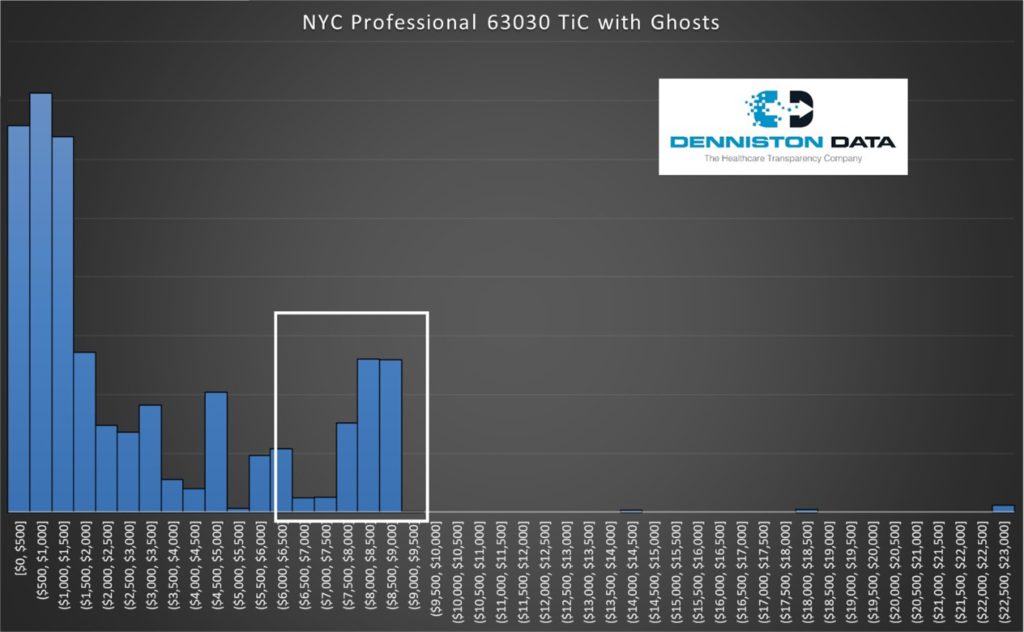
Ghost pricing is rampant in TiC data, and not unique to NYC. The biggest hole in the MRFs is they do not contain utilization data. How many times was the price paid to the doctor for the service? We see provider, procedure, and price, but if the doctor doesn’t do the procedure, don’t trust the price.
This means stakeholders need their own process using another data source or a trusted data analytics partner who can ascertain what’s real from what’s not.
This is particularly relevant for determining Qualifying Payment Amounts (QPAs) for out of network reimbursement, as evidenced by recent rulings in the Texas Medical Association’s suit challenging NSA on the presence of ghost rates. CMS defines QPA’s as the “median contracted rate”.
The recent Federal ruling states (page 43): “The Court holds that the following regulations are unlawful and must be set aside because they conflict with the No Surprises Act: (1) including in the calculation of QPAs contracted rates for services that providers have not provided…”
For lumbar discectomy in NYC, that changes the median from $1,500 to $8,250. Wowzah.
If your organization is negotiating, benchmarking, or settling on out-of-network QPAs using TiC files that have not been vetted against utilization, this phantom data will distort the pricing signals, creating a misleading picture of the actual costs associated with medical services.
That will cloud your decision-making and competitiveness, impairing the efficacy of the transparency initiative and its impact on the integrity of the healthcare system.
Conclusion
While the Transparency in Coverage Final Rule holds promise in revolutionizing the US healthcare landscape, the presence of ghost providers and inaccurate pricing threatens its effectiveness.
A threat, yes, but therein lies opportunity for those who can make sense of it. Stakeholders are rightly emboldened but must be cautious, vetting data sources to address this challenge, ensuring the transparency data reflects real utilization. Only through vigilant data-cleansing can the transparency initiative fulfill its intended purpose to empower decision-making and bring about positive change.
For more like this, join our email list at: https://www.dennistondata.com/email-list-form/
About the Author:
Phil LeFevre is Vice President of Business Development for Denniston Data Inc (DDI), and former Managing Director of ODG by MCG Health (where he remains in advisory capacity). Phil’s background at ODG was to unify evidence-based medicine with claims data analytics to improve outcomes and reduce friction, a relentless focus on workflow integration and customer experience. He brings these skills to DDI to help payers, providers, plan sponsors, and members identify the best doctors at the best prices by procedure, location, or plan using actual, negotiated rates and unbiased, data-driven quality metrics.
Disclaimer: The information contained in this article is provided for informational purposes only, and should not be construed as legal advice on any subject matter.
