Traditional methods for measuring physician quality in workers’ comp have used quality measures based on adverse events: mortality rates, hospital readmissions and, in terms of Workers Comp, delayed return to work. As such, the process for selecting WC Network Physicians, may unintentionally overlook providers who do a better job of treating injured workers impacted by Social Determinants of Health (SDOH). Why? Because injured workers with SDOH factors such as restricted access to care, low income or education, lack of transportation and housing are the workers most likely to experience adverse health outcomes. Providers treating that group are measured poorly – not due to the quality of their medical care, but because of adverse events coming from SDOH factors totally out of their control.
Author Archives: user
Transparency in Coverage Raw Data Files Can Ensure Employer Health Plans Are Paying Fair Prices
Self-insured employers have a new tool to ensure they are paying fair prices for medical services. The Consolidated Appropriations Act, 2021 (CAA) established protections for consumers related to surprise billing and transparency in health care. It created a unique opportunity by establishing the Transparency in Coverage (TiC) requirements, making available all negotiated prices from every healthcare payer to every medical provider for every service in the U.S., beginning in the latter half of 2022, updated monthly. These rules provided unprecedented access to proprietary price information.
Texas Prices Now Shown Separately in the Official Healthcare Pricing Guide Texas Release
Official Healthcare Pricing Guide (HPG) Can Ensure Employer Health Plans Are Paying Fair Prices Following the Consolidated Appropriations Act, 2021 (CAA)
Orthopedic Surgeons with Higher Surgical Volume Deliver Better Care Outcomes at Lower Costs
What is more important to you in choosing a doctor: (1) Bedside manner; or (2) Medical outcomes, i.e., success in performing a service that will get you better and/or keep you healthy? (4 minute read)
Former Leaders of ODG & MDGuidelines Launch Provider Ranking System™ to Find High Performing Providers for Workers’ Comp
Jon Seymour, MD Joins Denniston Data Inc. As Medical Director
While the “No Surprises Act” Failed to Hold Up in Court, Denniston Data Inc (DDI) Makes No Surprises Pact with Americans
Consumer Portal Identifies the Most Experienced Doctors by Procedure
Complimentary Consumer Portal from Denniston Data Inc. Identifies the Most Experienced Doctors by Procedure
Provider Ranking System™ (PRS) Adds latest CMS Data and new features to enhance user experience
Telehealth on upward trajectory – Are you ready?
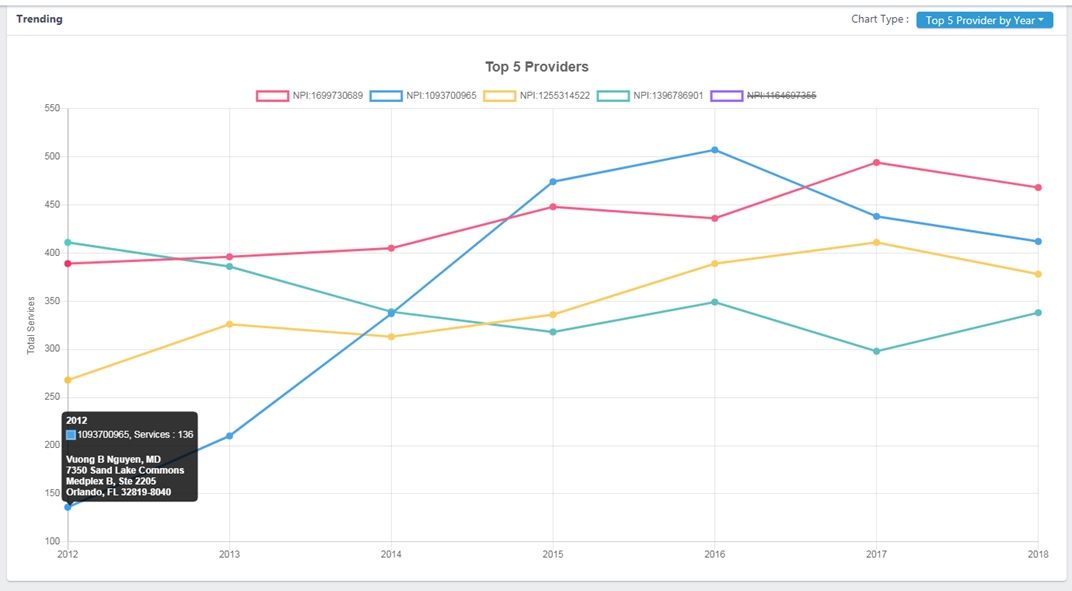
Many research and peer reviewed studies show that high-performing doctors produce better outcomes and cost less. Integrating evidence-based data of doctors’ practice experience like PRS into virtual health delivery platforms or health insurer’s provider network management system makes it easy for patients and professionals to find and access the best provider for their needs when and where they need the most, and at a more affordable cost.
Provider Ranking System™ (PRS) Launches Composite Ranking Score, Adds Enhanced Data Manipulation for AI
Provider Ranking System Brings Transparency to Healthcare Cost Dilemma
Did you happen to see the recent article from the New York Times titled, “Hospitals and Insurers Didn’t Want You to See These Prices. Here’s Why?” The August 2021, article is about how now a complete list of prices negotiated with private insurers, from every hospital, has been ordered from the federal government to be published.
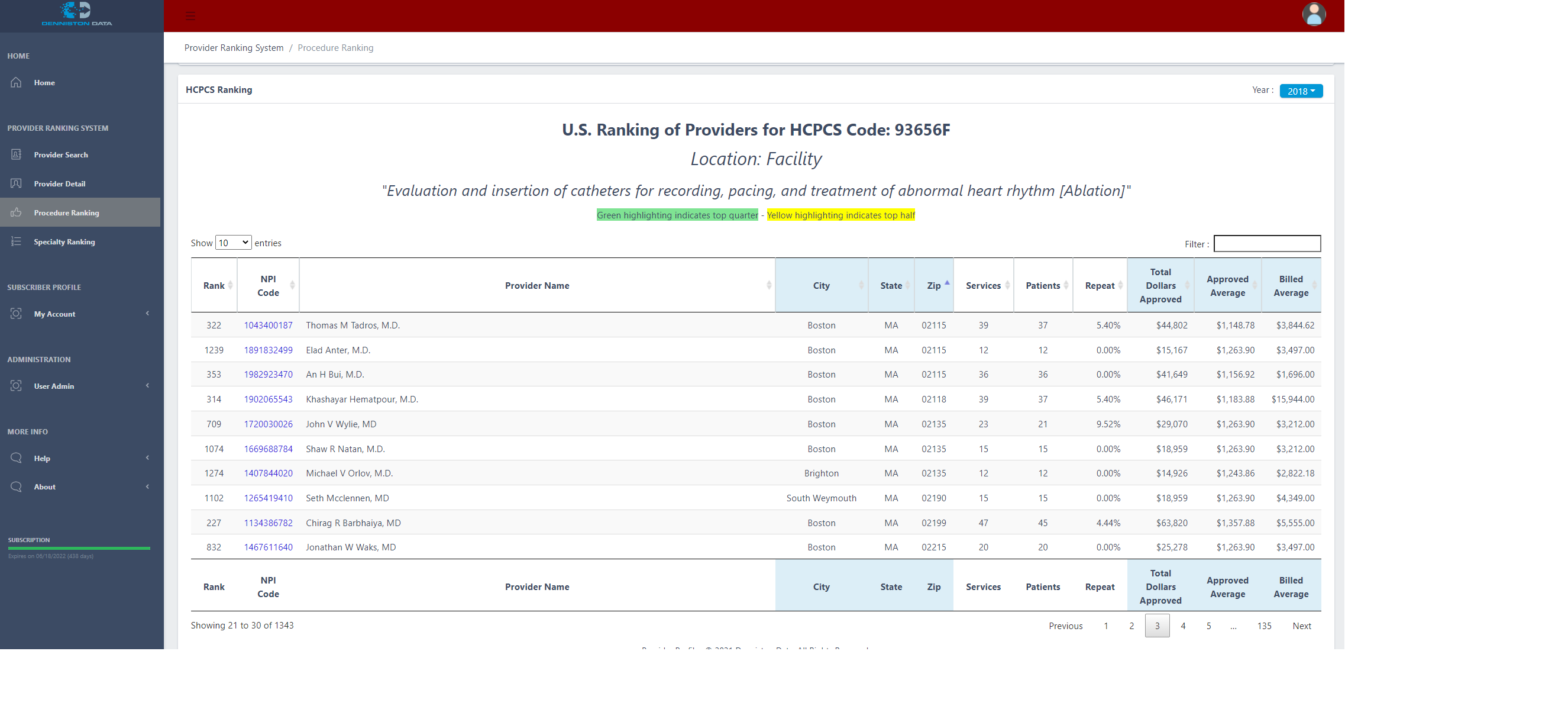
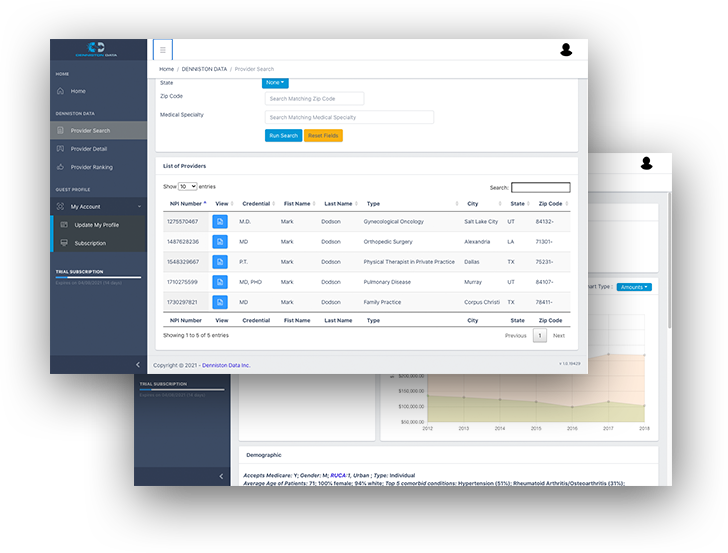
Provider Ranking System – How Does It Work?
Provider Ranking System (PRS) is designed for use by self-insured employers and health insurance companies to manage networks of providers, and to ensure that their employees or clients have access to the best doctors and other providers. View our online training demo and learn more.
Raising the Bar for Healthcare Providers
There is more to be gained by the release of Denniston Data’s Provider Ranking System, than the ability of users to find the most high-performing physicians…On a higher level, the very existence of an objective, transparent and annually updated ranking tool like PRS, serves a greater good.
How data is revolutionizing the way you access health information and research your doctors
When it comes to finding a medical provider, conducting your own due diligence is key. Whether it be individuals looking for healthcare providers, or professionals researching doctors, it is crucial to look beyond a provider’s resume and consult as many reliable resources as possible.
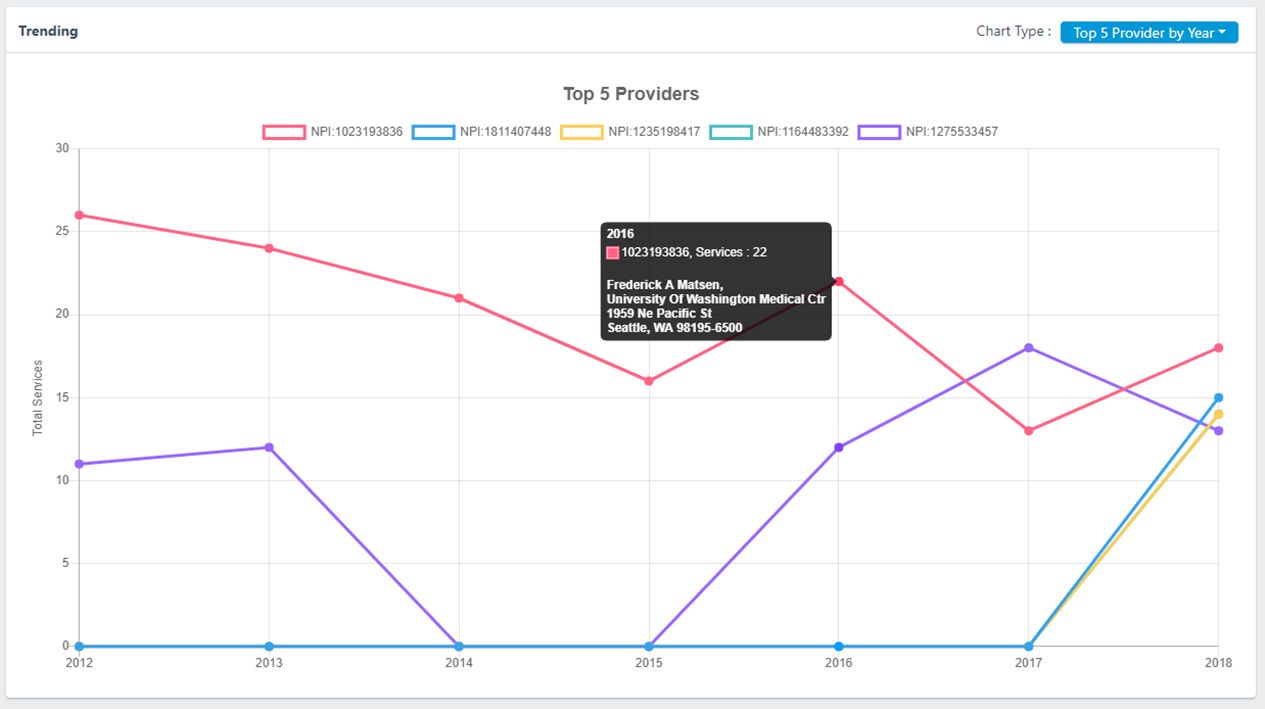
Finding the Right Shoulder Replacement Surgeon, a Case Study in How to Use the Provider Ranking System™ (PRS)
Patients who have a total shoulder arthroplasty or hemiarthroplasty performed by a high-volume surgeon or in a high-volume hospital are more likely to have a better outcome, including lowered mortality rates, postoperative complications, and hospital lengths of stay.
Denniston Data Inc. Launches Provider Ranking System to Compare Doctors by Experience Level
How to navigate doctor-finder services for healthcare
Knee Replacement Surgeons
Who are the Top Knee Replacement Surgeons in the United States based on Experience?
Does Practice Make Perfect in Healthcare?
What is more important to you in choosing a doctor: (1) Bedside manner; or (2) Medical outcomes, i.e., success in performing a service that will get you better and/or keep you healthy? (4 minute read)